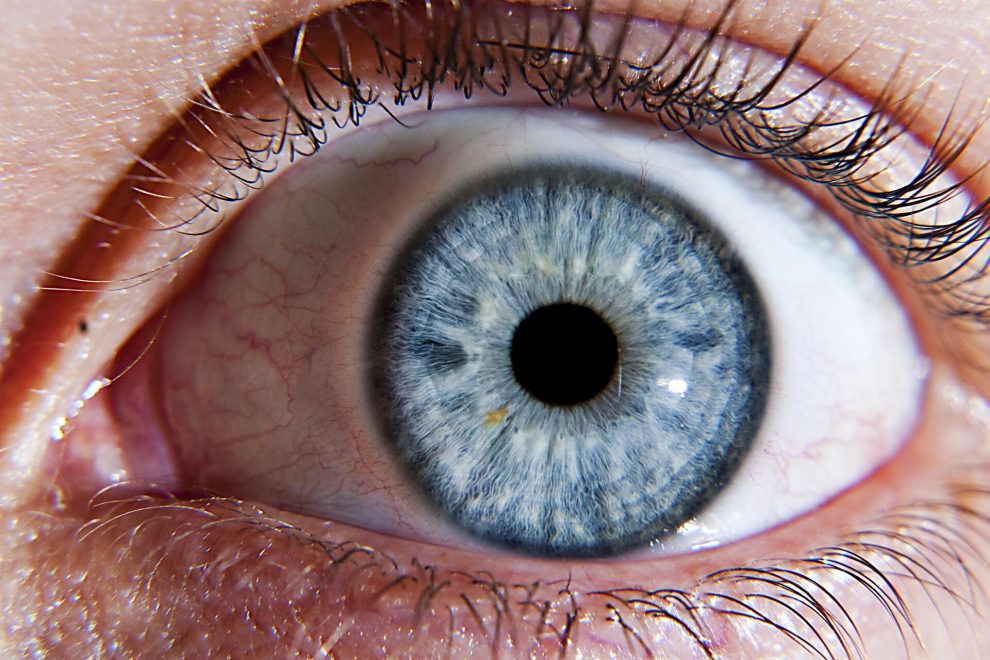
The dry eye (SOS) concept has been modified over the years, going from the initial name of keratoconjunctivitis sicca1 to the one agreed in April 2007 by the international dry eye working group lacrimal keratoconjunctivitis.2 It is defined as a multifactorial tear and ocular surface disease-causing symptoms of discomfort or discomfort, impaired visual acuity, and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear and inflammation of the ocular surface, caused by the loss of the homeostatic mechanism of the tear functional unit (UFL), which implies the formation of an unstable tear film that, finally, causes the symptoms dry eye.3
Its prevalence ranges between 10 and 20%, although it can rise to 33% in eastern populations.4 In Spain, the study carried out by Viso E. et al. Places the prevalence at 11%, more frequent in women than in men and significantly associated with aging. Although the symptoms have not been related to habits or systemic factors, they have been related to autoimmune diseases, acne rosacea, and the use of data display screens (PVD) .5
The dry eye symptoms affect the quality of life of those affected, and its high prevalence has an impact on health, care, and pharmacological costs. In Occupational Medicine – together with risk factors of a general nature, such as the use of contact lenses, refractive surgery, alterations of sex hormones, replacement therapy in menopause, bone marrow transplantation, or adverse effects of certain drugs (antiserotonergic, antidepressant, beta-blockers and the iatrogenic effects of chronic topical medication at the ocular level, such as eye drops that contain vasoconstrictors) —6 occupational risks must be assessed, among which radiation, low humidity, use of PVD and environmental pollutants, among others. .7
JOB RISKS, PROFESSIONS AFFECTED, AND DRY EYE SYNDROME
There are multiple occupational risk factors involved in SOS, but, without a doubt, the most studied are those related to work carried out with PVD and in offices. To better understand and understand the issues involved in this area, it is necessary to combine industrial hygiene approaches based on indoor air quality, occupational health approaches, and ophthalmology support.
With proper occupational factors, such as thermal factors (low relative humidity, high temperature) and demands related to the task performed (excess attention reduces blinking and enlarges the exposed ocular surface), the individual characteristics of each must be assessed. Worker (such as gland dysfunctions, the use of contact lenses, age, gender, and the use of certain medications) that, acting together, can cause this ocular discomfort due to alteration of the precorneal tear film (PTF). This alteration occurs by at least three mechanisms:
- The structure of the TFP is altered by a physical process that increases the rate of lost water emission resulting from hyperosmolarity, with dysfunction of the gland.
- The structural composition of the outermost lipid layer of the TFP is altered by aggressive aerosols and combustion products, both indoors and outdoors, facilitating water loss and possibly burning as a phenomenon of ocular hypersensitivity.
- Strong sensory irritant pollutants cause dry eyes by stimulating the trigeminal.
Also, exposure to some irritating chemical compounds and oxidative mixtures formed in the reactions between ozone and unsaturated organic compounds (alkenes) produces alteration of the TFP, and this effect can be exacerbated by low relative humidity in the air. 8
From a preventive point of view, the workplace, thermal conditions, the rhythm of the task, and the working day should be planned in a way that allows an adequate frequency of blinking and the realization of short and repeated pauses during the day to minimize alterations of the precorneal tear film.
Among the studies that have been carried out in recent years on this issue, the one carried out in 2003 by K. Skyberg and others in buildings in which no indoor air problems had previously been detected and in which the most severe symptoms stand out. Frequent symptoms reported by the workers were fatigue or heaviness of the head, irritation in the eyes, and dryness of the skin of the face, and the greatest affectation occurred in women. The risk was increased in workers with a previous allergy and in PVD users. Passive smoking and the psychosocial burden acted as predictors while improving the place’s cleanliness, ventilation system, and local temperature improved the clinic.
Dry Eye Syndrome affects more than 20% of the population from the age of 40
It is due to a production deficit or the low quality of the tear.
The use of artificial tears and humidifiers is essential to avoid visual fatigue and blurred vision.
What is dry eye syndrome, and why does it occur?
Dry eye syndrome is the set of ocular symptoms that produces a deficit in the number of tears due to decreased production or excessive evaporation. The low quality of the tear can also cause it.
What impact does it have, and which groups are more likely to develop it?
Dry eye syndrome is the first reason for consulting an ophthalmologist. More than 20% of those over 40 years of age suffer from it, being more frequent in women, and its incidence increases with age. It also increases the incidence in people who spend a lot of time reading or in front of the computer and dry environments.
How to know if you have dry eye and when should we go to the ophthalmologist’s office?
The symptoms of dry eye are:
Gritty or foreign body sensation in the eye
Burning in the eye
The feeling of heavy eyes
Visual fatigue
Blurry vision
We should go to a consultation when, despite using artificial tears, the symptoms do not improve, also when there is a pain in the eye or loss of vision.
Can dry eye syndrome be prevented?
In many cases, we cannot prevent dry eye, as it is due to hormonal alterations, age, or certain diseases. However, in other cases, where factors such as decreased blink frequency (reading, computer) or environmental dryness are involved, we can prevent it by using artificial tears and humidifiers.
What tests are done to diagnose it?
Two are carried out, the measurement of tear rupture time by staining the tear with an eye drop and the measurement of tear production through strips placed on the eyelid (Schirmer’s test). There are also other complementary tests for a chemical study of the tear.
What dry eye treatment options are there?
The treatment involves using artificial tears (various compounds and concentrations) and moisturizing gels or ointments.
There are also other options such as placing plugs in the tear points, certain oral medications, or the use of pulsed light.
How is the quality of life of a person with this pathology?
People who do not receive adequate treatment may see their daily activities, mainly visual, limited by discomfort, visual fatigue, and blurred vision. With treatment, the person can go about their daily activities without a problem.
What complications can occur?
In severe cases, they can cause severe inflammation and corneal scar formation with visual loss.



























Add Comment